Sickle-cell disease
Sickle-cell disease
Introduction
Sickle Cell Disease/ Anaemia
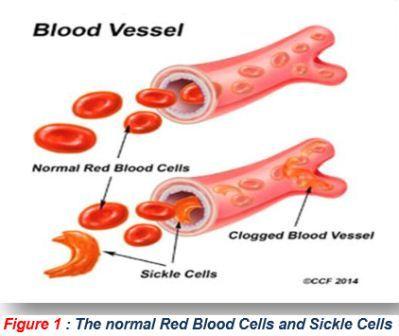
 Sickle cell disease (SCD) is a life threatening autosomal recessive genetic disorder resulting from inheritance of abnormal genes from both parents. Normal red blood cells (RBCs) are biconcave disc shaped and move smoothly through the blood capillaries. The RBCs are produced in bone marrow and average life of normal RBCs is about 120 days. Biconcave disc shape of RBCs changes to sickle shape under low oxygen tension due to polymerization of faulty haemoglobin called HbS arising out of a point mutation in beta globin gene. The life span of RBCs in SCD patients is only about 10 to 20 days and the bone marrow can't replace them fast enough. As a result there is decrease in number of RBCs in the body and the RBCs don’t contain sufficient amount of haemoglobin (hypochromia). In SCD the RBCs become sickle or crescent shaped which are stiff & sticky and tend to block the blood flow in small capillaries. Blocked blood flow causes ischemia leading to severe pain and gradual damage to organs.
Sickle cell disease (SCD) is a life threatening autosomal recessive genetic disorder resulting from inheritance of abnormal genes from both parents. Normal red blood cells (RBCs) are biconcave disc shaped and move smoothly through the blood capillaries. The RBCs are produced in bone marrow and average life of normal RBCs is about 120 days. Biconcave disc shape of RBCs changes to sickle shape under low oxygen tension due to polymerization of faulty haemoglobin called HbS arising out of a point mutation in beta globin gene. The life span of RBCs in SCD patients is only about 10 to 20 days and the bone marrow can't replace them fast enough. As a result there is decrease in number of RBCs in the body and the RBCs don’t contain sufficient amount of haemoglobin (hypochromia). In SCD the RBCs become sickle or crescent shaped which are stiff & sticky and tend to block the blood flow in small capillaries. Blocked blood flow causes ischemia leading to severe pain and gradual damage to organs.
Sickle cell gene is commonly believed to be associated with African ancestry and malaria endemic areas. Besides Africa, it is found around Mediterranean, Middle - East and India. The disease gene has spread also to Europe, America & Caribbean through migration of human populations.
Prevalence of SCD in India
In India, it is prevalent in States - Gujarat, Rajasthan, Uttarakhand, Maharashtra, Bihar, Jharkhand, Madhya Pradesh, Chhattisgarh, Odisha, West Bengal, Tamil Nadu, Telangana, Andhra Pradesh, Karnataka, Kerala, Uttar Pradesh & Assam.
Inheritance
Being an autosomal recessive disorder, abnormal beta globin gene from both mother and father are required to be inherited (homozygous) in offspring to cause SCD. If a person has only one abnormal beta globin gene inherited (heterozygous) either from mother or father, it is referred as sickle cell trait and are usually a symptomatic, but can pass the abnormal beta globin gene to their progeny
Situation
The Sickle cell anaemia has no available cure. However, treatments to improve the anaemia and lower complications can help with the symptoms and complications of the disease in both children and adults. Blood and marrow stem cell transplants may offer acure for a small number of people.
The Sickle cell anaemia varies from person to person. Some people who have the disease have chronic (long - term) pain or fatigue (tiredness). However, with proper care and treatment, many people who have the disease can have improved quality of life and reasonable health.
Because of improved treatments and care, people who have sickle cell anaemia are now living into their forties or fifties, or longer.
Pathophysiology
A single nucleotide substitution in the sixth codon of the ß globin gene results in the substitution of valine for glutamic acid on the surface of the variant-β globin chain. This change causes HbS to polymerise when deoxygenated, the primary event in all sickle cell pathology. Polymerisation is dependent on intra – erythrocytic HbS concentration, the degree of haemoglobin deoxygenation, pH and the intracellular concentration of HbF . The polymer is a rope – like fiber that aligns with others to form a bundle, distorting the red cell into characteristic sickled forms.
These deformed sickle red cells can occlude the micro vascular circulation producing vascular damage, organ infarcts, painful episodes and other symptoms associated with SCD.
There are two essential pathological processes: haemolysis and vaso - occlusion.
- Haemolysis results in anaemia and a functional deficiency of nitric oxide which results in vascular endothelial damage and may be responsible for complications such as pulmonary hypertension, priapism and stroke.
- Vaso – occlusion causes acute and chronic ischaemia and is responsible for acute pain and organ damage.
Sickle cell disease refers to not only patients with sickle cell anaemia but also to compound heterozygotes where one β globin gene mutation includes the sickle cell mutation and the second β globin allele includes a gene mutation other than the sickle cell mutation, such as mutations associated with HbC, HbS β - thalassemia, HbD, and HbO Arab. In sickle cell disease, HbS is >50% of total haemoglobin.
Sickle Cell Trait
People who inherit a sickle haemoglobin gene from one parent and a normal gene from the other parent have sickle cell trait. In sickle cell trait the HbS is <50% of total haemoglobin.
People who have sickle cell trait usually have few, if any, symptoms and lead normal lives. People who have sickle cell trait can pass the sickle haemoglobin gene to their children. The following image shows an example of an in heritance pattern for sickle cell trait.
Example of an Inheritance Pattern for sickle cell trait and disease

When both parents have a normal gene and an abnormal gene, each child has a 25 percent chance of inheriting two normal genes; a 50 percent chance of inheriting one normal gene and one abnormal gene; and a 25 percent chance of inheriting two abnormal genes
Symptoms
Signs and symptoms of sickle cell anemia often don't appear until an infant is at least 4 months old and may include:
- Anemia
- Episodes of pain
- Hand-foot syndrome
- Frequent infections
- Delayed growth
- Vision problems
- Fever
- Pale skin or nail beds
- Yellow tint
- Any signs or symptoms of stroke
Prevention of Sickle cell
- If both parents are carriers for sickle cell anemia, there is a 25% chance of a child being affected. Hence screening of couple before planning a child is very crucial. Screening for sickle cell anemia is possible by simple blood tests (point of care tests, CBC, HPLC, Electrophoresis, etc.).
- Ideally sickle cell status should be known prior to marriage.
- If not tested before marriage, all pregnant women should be tested in the first 3 months for both sickle cell anemia and thalassemia which is another
hemoglobin disorder that is common in India, using the same tests.
What should be done if diagnosed with Sickle Cell
- Routine follow-up visits with the doctor - at least once every 3 months or earlier as advised by the doctor
- Pneumococcal vaccination
- Consultation at the earliest in an event of crisis or any complication
- Possibility for curative treatment may be explored
Counseling for Diet Management
- Take a high fibre diet, plenty of roughage
- Take large amount of proteins in diet
- Choose diet rich in anti - oxidants
- Avoid oily and fatty foods (masala)
- Take plenty of water
Do’s & Dont’s
- Maintain a healthy lifestyle
- Drink plenty of water
- Modify dietary habits
- Be regular with their medicines.
- Take rest and relax
- Do not overwork. Avoid triggers like exhaustion, extreme cold, dehydration, high altitude and long-distance travel including long flights.
- Avoid extreme temperature
- Maintain hygiene to reduce the chance of infections
- Maintain regular schedules of work and play
Source: Sickle Cell Institute - Chhattisgarh
Related resources
Last Modified : 6/21/2024
Provides information about the initiative of deliv...
Provides information about World Sickle Cell Aware...
The National Sickle Cell Anaemia Elimination Missi...
