Psychosocial Triage
Psychosocial Triage
Triaging is a systematic assessment and classification of survivors to optimise and prioritise care based on their condition. It facilitates early identification and prompt mental health treatment for disaster-affected communities. Planning and arrangement of appropriate psychosocial support and mental health services can be done through psychosocial triage. This would not only reduce the consequences generated by disaster impact, but also ensure quality of psychosocial and mental health services. Psychological trauma is caused or worsened by the persons' closeness (physical or psychological) to the disaster, personal and environmental vulnerabilities, immediate and post disaster reactions and coping strategies/resources. Knowledge about these factors help frontline workers/community level workers/helpers to systematically code individuals affected by disasters as persons with low/medium/high risks and help them to decide upon what services to be given.
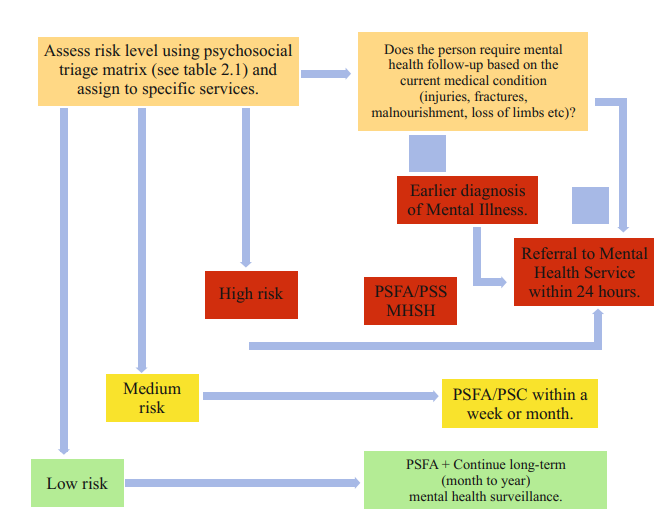
The psychosocial triage helps the caregiver to identify who requires immediate mental health attention, who has to be assigned for psychosocial care or PSFA and who has to be monitored by local health surveillance bodies.
Psychosocial triage matrix
| Indicators | Low Risk | Moderate Risk | High Risk |
| Physical closeness | Greater distance from the epicentre (disaster affected site). | Closer to the epicentre but not in the epicentre. | Present in the epicentre. |
| Expressive closeness | Does not know the survivor/s | Knows/friend to the survivor /s | Closely related or best friend of the survivor/s |
| Individual vulnerabilities |
|
|
|
| Environmental vulnerabilities |
|
|
|
| Instant reactions during the disaster | Appeared relaxed during the impact. | Expressed mild to moderate distress. | Expressed acute distress. |
| Ongoing reactions | Expressed few common crisis reactions. | Expressed many common crisis reactions. | Florid manifestation indicating mental health treatment (self-harm or causing harm to others, hyper vigilance, depression, acute dissociation, psychotic features, elated mood, etc.). |
| Coping | Active or adaptive coping (Able to deal with the impact effectively). | Uncertain coping (Unaware of how to deal with the impact). | Avoidant or Maladaptive coping (Harming self/others, use of substances). |
Source: Richter & Flowers 2008
Psychosocial Triage
To identify the persons who need psychosocial support, they need to be assessed based on their post-disaster reactions (excessive worry, fear, prolonged sadness, increased anger, sleep disturbance, disturbance in appetite etc.) and functioning (inability to perform everyday routine, lack of concentration in work, decreased quality of work, lack of interest in taking care of self, inability to socialise, interpersonal relationship issues, etc.).
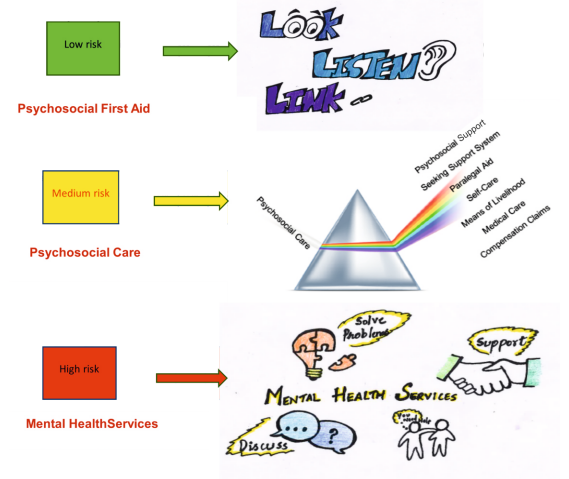
Based on the intensity of risk, the psychosocial support services need to be planned. For instance, persons who are at high risk, have to be referred to appropriate Mental Health Services within 24 hours. PSFA and PSS have to be provided within a week or month for the people who are at medium risk. For the low-risk people PSFA alone is sufficient. However, they have to be kept under mental health surveillance for a longterm (month to year).
Nature of psychosocial services provided based on the risk level
Case Illustrations in varied disasters
- “It was raining heavily for weeks. Houses, livelihoods and lives got swept away. The flood situation made me feel the lowest that I have ever felt in my life. I was afraid that I might lose my son”. A 42 years old mother affected by flood.
- “My family was traveling to our hometown for a wedding. I was busy with my work and could not join them. They left home by midnight. I woke up to hear the news of a bus crashing against a container. The news channels flashed saying 40 persons died including '4 members of a family'. I was praying hard that it was not mine. My life shattered in a flash”. A 35 years old husband.
- One day B, a nine years old girl woke up early in the morning hearing a crash and was told that a terrorist attack had taken place in the market. She took her teddy and rushed to check if Farina, her cook's daughter who loved her teddy was fine. She saw a tiny human drenched in blood. She kept the teddy next to her dead body. It has been two weeks already and she has not got out of her room even once. Whenever she hears a noise, she cries, shouting Farina.
- “There was a heavy pouring and forecast of landslide vulnerability, most people ere evacuated from the danger. The next day, the landslide hit the small-town causing loss of property and causalities. I could not reach my people as the telecommunication services in that area was affected.”. A 44 years old woman.
- C, a 22 years old visually challenged boy lost his entire family in the cyclone. He started questioning his existence asking himself whether he was a curse. He experienced feelings of grief, guilt and sadness. He wanted to kill himself, as he felt left out without any support. The only comfort was the dog that he adopted after the disaster.
- D, 34 years old police men worked in the frontline evacuation process during the Mangalore Air crash. He was staying away from his family and friends. After the first response with passengers, he felt traumatized seeing many lifeless passengers who lost their lives. He started losing interest in his daily activities, experienced disturbances in sleep and appeared to be moody and irritable. He complained of stress because of heightened societal pressure to aid the needy.
Last Modified : 11/23/2023
Tips for handling mental issues during pandemics/d...
MANODARPAN initiative of Ministry of Education is...
This topic provides information about the importan...
World Suicide Prevention Day (WSPD), on 10 Septemb...
