Revised Comprehensive Guidelines for Management of COVID-19 in Children and Adolescents
Revised Comprehensive Guidelines for Management of COVID-19 in Children and Adolescents
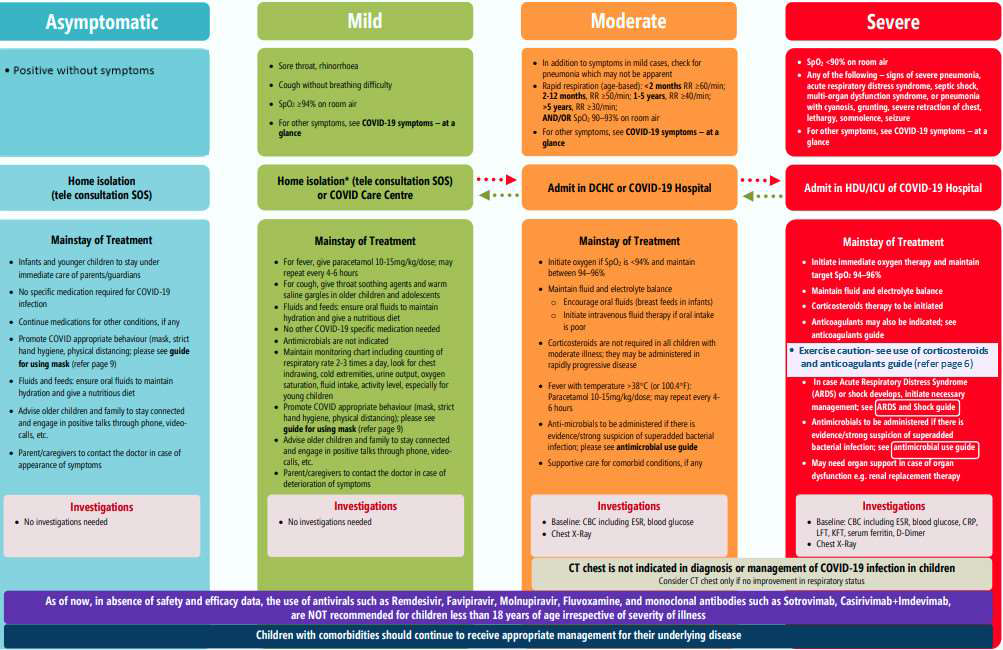
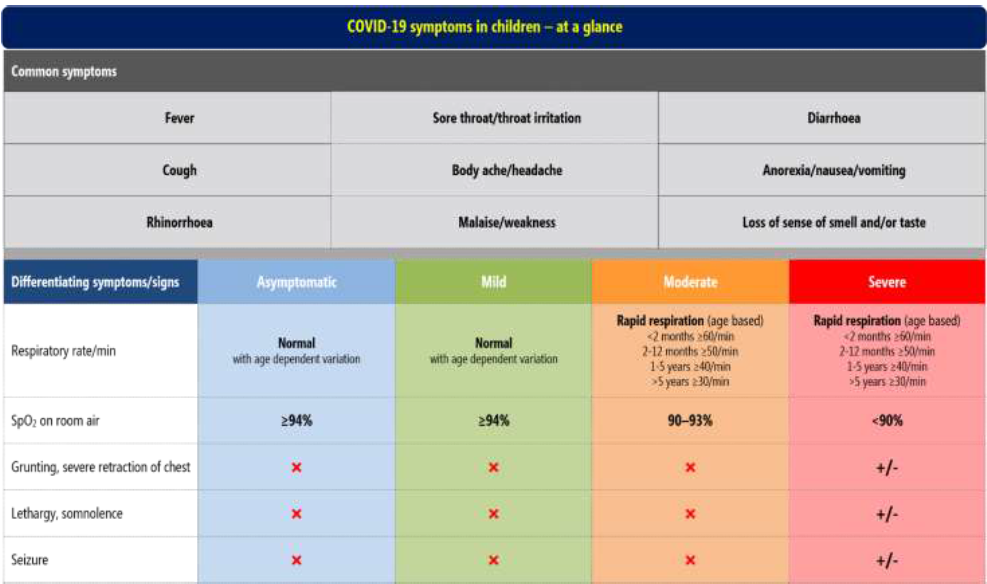
- COVID-19 symptoms in children – at a glance
- Management of Acute Respiratory Distress Syndrome (ARDS) and Shock guide
- Management of Multisystem Inflammatory Syndrome (MIS-C) in children and adolescents temporally related to COVID-19
- Infection Prevention and Control (IPC)
- Guide for using mask
- Antimicrobial use guide
- Use of steroids and anticoagulants
- Post COVID Care
COVID-19 symptoms in children – at a glance
The Comprehensive Guidelines for Management of COVID-19 in CHILDREN and ADOLESCENTS (below 18 years) were reviewed by the group of experts in view of the current surge mainly attributed to the Omicron variant of concern. The available data from other countries suggests that disease caused by the Omicron variant is less severe; however, there is need for a careful watch, as the current wave evolves. These guidelines are dynamic, and will be reviewed and updated, on availability of new evidence.
The experts have assessed the available evidence and overall, the management remains unchanged, barring a few changes outlined below.
- Title of the document has been changed from Comprehensive Guidelines for Management of COVID-19 in CHILDREN (below 18 years) to Comprehensive Guidelines for Management of COVID-19 in CHILDREN and ADOLESCENTS (below 18 years).
- Use of antivirals or monoclonal antibodies is not recommended for children less than 18 years of age, irrespective of the severity of infection.
- For diagnosing MIS-C, caution should be exercised while interpreting an isolated increase in COVID antibodies.
- The CRP level for diagnosis of MIS-C has been revised as >5mg/dL.
- If steroids are used, they should be tapered over 10-14 days, subject to clinical improvement.
- Use of anticoagulants has been revised.
- New section on post-COVID care has been added.
Attention is drawn to the following MoHFW guidelines:
- FAQs on SARS-CoV-2 Variant-Omicron
- Revised guidelines for Home Isolation of mild /asymptomatic COVID-19 cases
- Guidelines for COVID-19 Vaccination of Children between 15 to 18 years and Precaution Dose to HCWs, FLWs & 60+ population with comorbidities
COVID Appropriate Behavior is recommended to prevent SARS-CoV-2 infections:
3Ws:
- Watch your distance (more than 2 meters)
- Wash your hands
- Wear a mask
2Vs:
- Ventilation – open spaces are less risky than closed or poorly ventilated areas
- Vaccination – for 15-18 years age group
Management of Acute Respiratory Distress Syndrome (ARDS) and Shock guide
Management/treatment of ARDS
ARDS may be classified based on Pediatric Acute Lung Injury Consensus Conference (PALICC) definition into mild, moderate and severe
Mild ARDS
- High flow nasal oxygen (start with 0.5 L/kg/min to begin with and increase to 2 L/kg/min with monitoring) or non-invasive ventilation (BiPAP or CPAP) may be given
Moderate – Severe ARDS
- Lung protective mechanical ventilation may be initiated; low tidal volume (4-8 ml/kg); plateau pressure <28-30 cmH2O; MAP <18-20 cmH2O; driving pressure <15 cmH2O; PEEP 6-10 cmH2O (or higher if severe ARDS); FiO2 <60%; sedoanalgesia ± neuromuscular blockers; cuffed ETT, inline suction, heat and moisture exchange filters (HMEF)
- Avoid frequent disconnection of ventilator circuit, nebulization or metered dose inhaler
- Restrict fluids; calculate fluid overload percentage, keeping it <10%
- Prone position may be considered in hypoxemic children if they are able to tolerate it
- Daily assessment for weaning and early extubation; enteral nutrition within 24 hours, achieve full feeds by 48 hours
- Transfusion trigger Hb <7g/dL if stable oxygenation and haemodynamics and <10 g/dL if refractory hypoxemia or shock
Management of shock
- Consider crystalloid fluid bolus 10-20 ml/kg cautiously over 30-60 minutes with early vasoactive support (epinephrine)
- Start antimicrobials within the first hour, after taking blood cultures, according to hospital antibiogram or treatment guidelines
- Consider inotropes (milrinone or dobutamine) if poor perfusion and myocardial dysfunction persists despite fluid boluses, vasoactive drugs and achievement of target mean arterial pressure
- Hydrocortisone may be added if there is fluid refractory catecholamine resistant shock (avoid if already on dexamethasone or methylprednisolone)
- Once stabilized, restrict IV fluids to avoid fluid overload
- Initiate enteral nutrition – sooner the better
- Transfusion trigger Hb <7g/dL if stable oxygenation and haemodynamics, and <10 g/dL if refractory hypoxemia or shock
Management of Multisystem Inflammatory Syndrome (MIS-C) in children and adolescents temporally related to COVID-19
Multi System Inflammatory Syndrome in Children (MIS-C) is a new syndrome in children characterized by unremitting fever >38oC and epidemiological linkage with SARS-CoV-2.
Diagnostic criteria (WHO)
- Children and adolescents 0–18 years of age with fever ≥3 days
- And any two of the following:
- Rash or bilateral non-purulent conjunctivitis or muco-cutaneous inflammation signs (oral, hands or feet)
- Hypotension or shock
- Features of myocardial dysfunction, pericarditis, valvulitis, or coronary abnormalities (including ECHO findings or elevated Troponin/NT-proBNP)
- Evidence of coagulopathy (PT, PTT, elevated D-Dimers)
- Acute gastrointestinal problems (diarrhoea, vomiting, or abdominal pain)
- And elevated markers of inflammation such as ESR (>40 mm), C-reactive protein (>5 mg/L), or procalcitonin
- And no other obvious microbial cause of inflammation, including bacterial sepsis, staphylococcal or streptococcal shock syndromes
- And evidence of recent COVID-19 infection (RT-PCR, antigen test or serology positive), or likely contact with patients with COVID-19
Alternative diagnoses that must be excluded before making a diagnosis of MIS-C
- Tropical fevers (malaria, dengue, scrub typhus, enteric fever)
- Toxic shock syndrome (staphylococcal or streptococcal)
- Bacterial sepsis
MIS-C with Kawasaki Disease (KD) phenotype is characterised by fever, conjunctival redness, oropharyngeal findings (red and/or cracked lips, strawberry tongue), rash, swollen and/or erythematous hands and feet and cervical lymphadenopathy
To know information about Stepwise investigations in a patient with MIS-C and Management of MIS-C Click Here.
- Appropriate supportive care is needed preferably in ICU for treatment of cardiac dysfunction, coronary involvement, shock or multi-organ dysfunction syndrome (MODS)
- IVIG to be given slower (over up to 48 hours) in children with cardiac failure/ fluid overload
- Use biologicals only after expert consultation and at tertiary care only
- Taper steroids over 2-3 weeks with clinical and CRP monitoring
- Aspirin 3-5 mg/kg/day, maximum 75 mg/day in all children for 4-6 weeks (with platelet count >80,000/µL) for at least 4-6 weeks or longer for those with coronary aneurysms
- Low molecular weight heparin (Enoxaparin) 1 mg/kg/dose twice daily s/c in >2 months (0.75mg/kg/dose in <2 months) if patient has thrombosis or giant aneurysm with absolute coronary diameter ≥8 mm or Z score ≥10 or LVEF <30%
- For children with cardiac involvement, repeat ECG 48 hourly & repeat ECHO at 7–14 days and between 4 to 6 weeks, and after 1 year if initial ECHO was abnormal
Infection Prevention and Control (IPC)
Every COVID care facility should have a multidisciplinary hospital infection control committee; key components of infection control strategy are:
- Standard precautions
- Droplet precautions
- Airborne precautions
- Contact precautions and hand hygiene
- Physical distancing
- Cough etiquette/respiratory hygiene
- Well ventilated rooms
- Monitor healthcare associated infections
- Train all health care workers to develop IPC skills
- Environment cleaning, disinfection and sanitation
- Cleaning/disinfection of frequently touched surfaces/equipment
- Cleaning and disinfection of linen
- Safe management of bio-medical waste
- Triple layer mask to be worn by patient, as per guidance below
- Masks for care givers (home/hospital)
Guide for using mask
- Masks are not recommended for children aged 5 years and under
- Children aged 6-11 years may wear a mask depending on the ability of child to use a mask safely and appropriately under direct supervision of parents/guardians
- Children aged 12 years and over should wear a mask under the same conditions as adults
- Ensure hands are kept clean with soap and water, or an alcohol-based hand rub, while handling masks
Antimicrobial use guide
COVID-19 is a viral infection, and antimicrobials have no role in the management of uncomplicated COVID-19 infection
- Asymptomatic and mild cases: antimicrobials are not recommended for therapy or prophylaxis
- Moderate and severe cases: antimicrobials should not be prescribed unless there is clinical suspicion of a superadded infection
- Septic shock: empirical antimicrobials (according to body weight) are frequently added to cover all likely pathogens based on clinical judgement, patient host factors, local epidemiology and antimicrobial policy of the hospital
Use of steroids and anticoagulants
Steroids
- Steroids are not indicated and are harmful in asymptomatic and mild cases of COVID-19
- Indicated only in hospitalized severe and critically ill COVID-19 cases (Under Strict Supervision)
- Steroids should be used at the right time, in right dose and for the right duration
- Indications and recommended dose of corticosteroids – may be used in rapidly progressive moderate and all severe cases
- Dexamethasone 0.15 mg/kg, maximum dose 6 mg once a day OR
- Methylprednisolone 0.75 mg/kg, maximum dose 30 mg once a day
- Continue for 5-7 days and taper, up to 14 days, depending on clinical assessment on daily basis
- Avoid steroids in first 3-5 days since onset of symptoms as it prolongs viral shedding
Anticoagulants
- Not indicated routinely
- All hospitalized children should be monitored for thrombosis; on suspicion, confirm by appropriate investigations and start on low molecular weight heparin in therapeutic doses for period of 12 weeks with monitoring
- Prophylactic anticoagulant is indicated in following circumstances (the decision to administer prophylactic anticoagulation must be balanced with the child's bleeding risk):
- strong personal or family history of VTE
- an indwelling central venous line and two or more additional risk factors
- four or more risk factors
- (*Predisposing risk factors for development of thrombosis – personal history of venous thrombotic events (VTE), family history of first-degree relative with VTE, presence of central venous line, decreased mobility from baseline, burns, active malignancy, estrogen therapy, flare of inflammatory disease, morbid obesity, severe dehydration, recent surgery or trauma)
- Prophylactic dose of low molecular weight heparin (Enoxaparin): 0.5 mg/kg twice daily, till child is discharged from hospital
- On suspicion of thrombosis, confirm by appropriate investigations and start on low molecular weight heparin in therapeutic doses for period of 12 weeks with monitoring
- Children already on anticoagulation therapy may continue same unless they develop active bleeding
- Therapeutic dose of low molecular weight heparin (Enoxaparin): 1 mg/kg twice daily
Post COVID Care
- Children with asymptomatic infection or mild disease should receive routine childcare, appropriate vaccination (if eligible), nutrition counselling, and psychological support on follow up
- In addition to above, for children with moderate to severe COVID, at discharge from hospital, parents/caregivers should be counselled regarding monitoring for persistence/worsening respiratory difficulty and explained the indications for bringing the child back to facility
- Children who develop any organ specific dysfunction during hospital stay or subsequently should receive appropriate care
Source : Ministry of Health & Family Welfare
Last Modified : 12/26/2023
MoHFW released Guide to address stigma associated ...
ICMR's Guidance for Management of Pregnant Women i...
The topic provides information related to Minding ...
This topic provides information about Coronavirus.
